Ocular Surface Squamous Neoplasia (abbreviated as OSSN) is comprised of a vast array of conjunctival and corneal lesions which runs from dysplastic lesions and extends towards invasive squamous cell carcinoma. On a general note, this sort of tumor is often categorized as a low-grade malignancy; however, it should be noted that invasive lesions could proliferate and reach the globe/orbit. OSSN is recognized ubiquitously as a malignancy of the cornea and conjunctiva.
Over the course of the past few years, the treatment of OSSN has undergone substantial changes – in a constructive sense – which were induced by a more comprehensive knowledge of the disease, consolidation of diagnostic capacities of the diseases, as well as a major tilt towards better-structured management medical of the tumors. As it stands, there exists an improved level of orientation pertaining to the topics of its association with solar exposure and other conditions like xeroderma pigmentosa, and HIV infection.
For OSSN, risk factors can either be environmental or genetic. Exposure to ultraviolet (UV) radiation is considered the greatest risk factor when it comes to OSSN. Just as is the case with cutaneous malignancies, UV radiation causes carcinogenesis and detrimental effects to DNA in the same vein. Conversely, with the genetic aspect of the risk factors, individuals having genetic disorders such as xeroderma pigmentosa have a greater propensity of suffering UV radiation-begotten damage to their cells, as a consequence of lack of capacity to correct mutations in the DNA, and to that effect, are at a greater risk of the ocular surface and cutaneous malignancies. The Human Papilloma Virus (HPV) is another risk factor of OSSN worthy of mention; carcinogenesis induced by HPV has been greatly ascribed to the capability of its oncoproteins, E6 and E7 to be specific, to single out and associate with host cellular proteins, take p53 for instance, and catalyze the degradation of normal proteins. As seen with HIV and atopy/allergy, local and systemic immunosuppression are constantly being linked with OSSN, most probably as a result of the tumor-recognition capabilities of the immune cells being impaired. However, an association of other factors has been found with this condition, such factors include but are not limited to old age, male sex, fair skin pigmentation, heavy smoking of cigarettes, continued exposure to petroleum products.
To begin with, clinical features of the lesion such as morphology, size, site, surface, feeder vessels, as well as the precise anatomical location whether it is scleral (pivoted to the globe) or conjunctival involvement should be investigated. A proper evaluation of the extension of lesions should be conducted.
Gonioscopy should be carried out to evaluate the invasion angle of the tumor; on the other hand, dilated fundus examination should be conducted to weigh up the intraocular invasion. Be that as it may, in circumstances involving media opacity, B-Scan ultrasonography could prove vital in the process of assessing intraocular spread and the sclera as a whole.
By way of CT or MRI scans, the precision and extension of the mass could be used to precisely evaluate the nature of orbital or anterior eye involvement.
As a section of the clinical examination, it is of great significance to look into the regional lymph nodes as well (both preauricular, cervical, and submandibular lymph nodes).
However, since mere clinical appearance might not do justice to the discrepancies between intraepithelial and invasive lesions, it is strongly recommended that tissue histology – which can either be conducted using incisional or excisional biopsy – be employed for a definite diagnosis.
When dealing with relatively small tumors (not more than 4 clock hours of limbal involvement or not exceeding 15mm of basal diameter — could be less in any case), excisional biopsy is generally chosen above incisional biopsy. Lesions that are greater in size could be attended to with the wedge or punch biopsy. In addition, Incisional biopsy is well suited for conditions whose ideal remedies come in form of topical chemotherapy or other treatments like radiation.
The histologic features of OSSN can be categorized based on the presence of dysplastic cells which originate from the basal cell layers that extend towards the surface. The patterns/configurations of dysplastic changes are quite numerous, and vary from the small squamous cells with augmented nuclear-cytoplasmic ratio, large squamous cells with hyperchromatic nuclei, and of course spindle cells having oval-shaped nuclei. With either anisonucleosis or nuclear pleomorphism, the dysplastic cells are taken to be composed of anomalous nuclei. Furthermore, mitotic figures are seen to rise and gradually shifted up towards the surface, together with the degree of dysplasia; a lot of mitotic figures are aberrant.
Treatment for OSSN can be administered surgically or by non surgical means, or in some cases, a combination of both; depending on the individual patient. Medical non-surgical treatments come in form of eyedrops, topical Mitomycin-C, 5-fluorouracil and Interferon Alpha 2b. The aforementioned medications are beneficial in the sense that they treat the ocular surface, in toto, for any anomalous cells and oftentimes do not need to be followed up with surgical intervention. However, with the use of these medications, compliance is paramount, as it is imperative that they be taken over periods spanning weeks or months. Mitomycin-C (MMC) is a drug used in the treatment of certain forms of cancer, and also for the alleviation of post-surgical scarring; and to this end, has been employed in the treatment of OSSN, especially in the past decade. In cases of stubborn tumors or failure of surgery to eradicate the tumor in toto, the MMC is applied.
Per contra, surgical treatment is considered the traditional approach to the treatment of OSSN. The process of surgical excision entails the resection of the OSSN from the eye surface, leaving behind a healthy margin of tissue, and the lesion is sent out for pathology testing. It is demanded that follow-up visits are scheduled to keep watch for any indications of recurrence.
Surgical excision is the ideal form of treatment for certain classes of patients, such as patients with large tumors, and/or an indefinite diagnosis.
The resection of the tumour is done with a 1:1 mixture of 2 percent lidocaine and 0.75 percent bupivacaine for local peribulbar or retrobulbar anesthesia. To bring about vasoconstriction, phenylephrine 2.5 percent drops are used; by so doing, perioperative bleeding is reduced and better visualization of the tumor’s corneal progression is enabled. Subsequent to delineating the tumor’s borders, calipers are used to mark 4-mm margins at the edges of the sclera. Forceps are used to raise the conjunctiva, thereafter Westcott scissors are used to create the first incision. To prevent tumor seeding, the first tumor dissection is limited to the made margins, and any form of contact of the tumor with surgical equipment is avoided. Upon the successful completion of dissecting the localized marked margins, the dissection is thence directed along a path towards the core of the tumor. A partial-thickness sclerectomy is conducted using a blade and forceps if in case the tumor happens to cleave to the sclera. After the removal of the lesion as a whole, the specimen is marked in the orientation specified with sutures and then carried on to a piece of pencil-marked cardboard, as is. The specimen is afterward passed on to pathology in formalin.
Absolute alcohol epitheliectomy is carried out if corneal involvement exists. A scrupulous schematic is drawn at the slit lamp to adequately envisage the corneal involvement. Additionally, as the surgery goes on, the pupil maybe dilated to allow optimal visualization of the corneal involvement in the operating room. The devitalized epithelium is scraped off with relative ease, leaving 3–4 mm of safety margins that bear similitude with the conjunctiva.
These cells are placed inside a cellulose sponge and are sent out to a histopathologist to evaluate them.
The limbus and sclera bed are scraped as well, and the lesion’s limbus and conjunctival margins are then frozen. What follows is the cauterization of the scleral bed. Hence, hemostasis is established, and any prospective remnant tumor cells may be rendered nonviable. To prevent damage to the sclera and underlying retina, a twofold freeze-thaw cycle is implemented at the limbus, and the conjunctiva is pulled away from the sclera bed. The bipartite freeze-and-slow-thaw cryotherapy approach harms cells by forming intracellular ice crystals and inducing ischemic necrosis in cells that have already been frozen. To avoid tumor seeding, the conjunctival defect is covered up with an amniotic membrane transplant using new equipment. The stromal side of the amniotic membrane is placed down upon the conjunctival defect and fibrin glue is put underneath the membrane to bind it to the underlying sclera. The amniotic membrane is smoothed with the aid of a muscle hook. To assuage discomfort, tissue glue is put to the corneal defect in droplets. Instead of sutures, the amniotic membrane combined with tissue glue decreases inflammation, promotes epithelialization, and avoids neovascularization.
The preference of amniotic membrane along with tissue glue over sutures helps to reduce inflammation, prevent neovascularization, and at the same time, promote epithelialization.
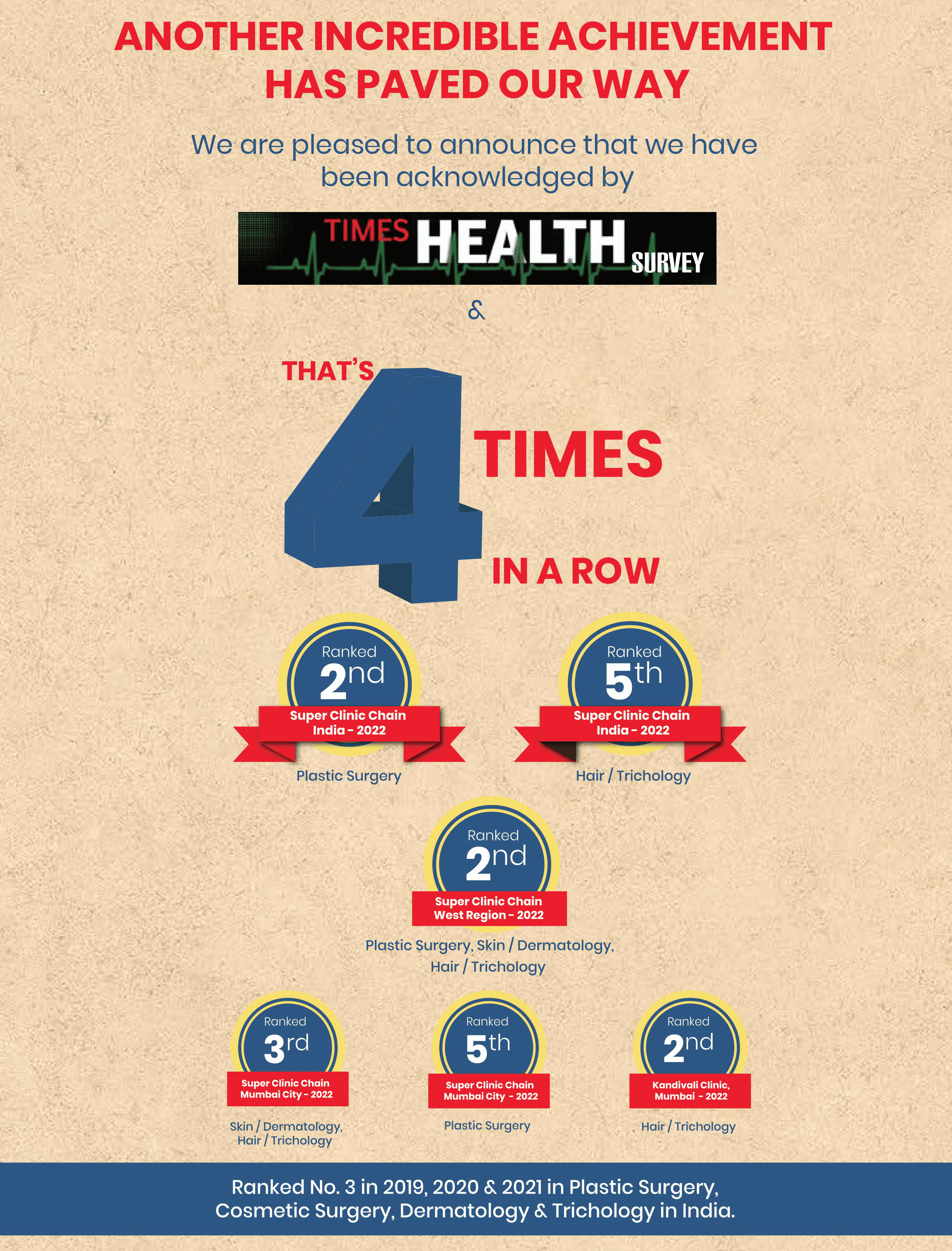
With an operation as sophisticated as the surgery for OSSN, it is imperative that it be conducted under the aegis of an exquisite team of plastic surgeons, who have various years of experience in their locker in the field. At The Esthetic Clinics, where Dr. Debraj Shome — India’s Celebrity Oculoplastic surgeon who has numerous accolades to his name — heads an expert group of cosmetic surgeons and plastic surgeons. To top it off, the medical facility available in our facility is primed to ensure the success of your Ocular Surface Squamous Neoplasia surgery, right from the pre-operative to post-operative phase, you can place your trust in us.
When it comes to determining the cost of OSSN surgery, it's critical that we get a firsthand look at your situation so we can give you an accurate estimate. The cost of an OSSN surgery procedure is determined by the extent of the defect, the diagnosis, the surgeon's fee, prescriptions, and the length of follow-up.


Dr. Debraj Shome is Director and Co founder of The Esthetic Clinics. He has been rated amongst the top surgeons in India by multiple agencies. The Esthetic Clinics patients include many international and national celebrities who prefer to opt for facial cosmetic surgery and facial plastic surgery in Mumbai because The Esthetic Clinics has its headquarters there.