Exenteration – or orbital exenteration – is a surgical process that entails the resection of the eyeball and the tissues by which it is encompassed; such include the muscles, nerves, fatty tissues adjacent to the eye, and the eyelids (the degree of removal would be determined by what disease is being treated). Exenteration could either be total, subtotal or extended. By convention, the exenteration procedure is comprised of the excision of the conjunctiva, eyelids, the globe, and the orbital contents in their totality, which is inclusive of the periorbita.
Furthermore, Superexenteration, which is otherwise referred to as extended exenteration, might involve the bony orbital walls, adjacent paranasal sinus tissues, and/or intracranial tissue. Subtotal exenteration, on the other hand, is concerned with the removal of the conjunctiva, the globe, and extraocular muscles and subperiosteal dissection. When one considers the proper preservation of orbital tissue volume, eyelids, or conjunctiva, subtotal exenteration has an inclination to facilitate the use of orbital or ocular prosthesis. This, in turn, helps speed up the rate of healing, comes with much less complications, fewer modifications to the dressings made, and at the same time enhances functional and esthetic results.
Every patient being put forward for exenteration surgery should be assessed in a preoperative manner, by a head and neck surgeon or ophthalmologist; in events where there is involvement of the skull base, a neurosurgical evaluation has to be conducted. On the other hand, for patients set aside for reconstruction, their examination should be conducted as due, by a reconstructive plastic surgeon. A radiological assessment is comprised of two aspects, the magnetic resonance imaging part — which is augmented using gadolinium — and a high resolution contrast-enhanced computed tomographic scan (CT scan). On one hand, the MRI provides an enumeration of intracranial and orbital involvement, and conversely, the CT scan offers an ideal representation of bony structures. In a bid to come out with more accurate staging, the examination is conducted on patients with malignant tumors on the basis of tomographic CT (PET-CT). By so doing, the surgical process and treatment are made much more straightforward as redundant processes are cut out when it concerns patients with distant metastases. Having stated that, if the metastatic disease of the patient is ascertained, the survival benefit should be juxtaposed against the morbidity of exenteration.
Once the necessary examinations have been completed in the diagnostic phase, the next aspect will be about preparing for the surgery – after the date must have been fixed. The surgeon will provide you with extensive details on the procedure and also see to it that your mind is prepared to live with the loss of vision – on the eye(s) that would be operated on.
Again, you should note that medications such as blood-thinning and immunosuppressive drugs should be discontinued weeks before your orbit is exenterated – make sure you show the surgeon the medications you are using at the time of your first appointment. Additionally, you are not expected to eat anything six hours before your exenteration surgery.
There are a number of risks associated with exenteration surgery; some of these include:
The potential complications of exenteration yet give an insight into how complex it is, and this is the very reason you should consider having your surgery in a top clinic with the right resources and the best team of surgeons to perform the procedure on you.
Orbital exenteration is, more often than not, done under general anesthesia; be that as it may, for older patients with comorbidities, intravenous sedation with local anesthetic has been reported.
To get proper traction of the orbital contents, either skin sutures or a large-sized Allis clamp are routinely applied to the lid edges. Overlying the bone rim of the orbit, a circumferential skin incision is marked out or ascribed. At the initial stage, the skin is incised with a cold knife, then monopolar cautery up until the periosteum is reached successfully. The supraorbital nerve is carefully preserved in order to maintain sensation in the forehead. Save for the tight attachment of the medial and lateral canthal ligaments and the trochlea, which is best destroyed with a No. 15 blade scalpel, the periorbita separates readily temporally, above, and medially.
The thinness of the orbital roof should be properly set out so that the anterior cranial cavity is not penetrated inadvertently. As a consequence of the thinness of the nasal orbital wall over the ethmoid air cells, meticulous attention must be given to the process of elevating the periorbita to avoid opening into the nasal cavity. The anterior and posterior ethmoidal arteries are ligated and transected upon the removal of the lacrimal sac.
The neoplasm may be discovered during the separation of the periorbita along the rim or the orbital wall. As far back as the apical stump and along the superior and inferior fissures, the periorbita can be released. Monopolar cautery can be applied as a technique to clamp and cauterize the above.
Curved neurectomy scissors applied with expertise from the nasal end can be used to cut the apical stump. To prevent bleeding, the stump will almost always require further clamping and cauterization. The orbital apex’s ocular muscles, optic nerve, and ophthalmic arteries are then transected. A rongeur is utilized to remove the involved bone and bone wax might be used to stop bleeding. The orbit is now packed, and the patient can proceed with their preferred reconstructive approach.
Going by the invasiveness of exenteration; it is usually more challenging to manage the orbit thereof. Owing to this, the best exenteration procedural routine will include engaging the services of an experienced ocularist to prepare the prosthesis to place in the orbit after the surgery has been completed.
It is strongly recommended to the patients that the skin surrounding the incision be cleaned with cool, boiling water; the rest of the face can be cleansed as you would on a normal day. Patients should avoid the blowing of their noses and try to lessen vehement sneezing for 6 weeks following surgery, this is just for the reason that socket is adjacent to the air sinuses. This reduces the chance of air entering the socket and causing subsequent infection. On a closing note, sleeping with the head elevated on two extra pillows for two weeks helps to reduce bruising and swelling.
An ocular prosthesis, made of silicone, created as a replica of the other eye, is constructed to improve the cosmetic look. This can be attached to the socket with specialized magnetic implants or fixed to a pair of glasses. These prostheses are oftentimes handcrafted by a professional and usually have a very pleasing overall visual look.
All patients will require ongoing clinical monitoring for up to 5 years, as well as adjuvant local radiation and/or chemotherapy (after the socket has settled). This is organized by an oncologist with experience in the field and is thought to ‘mop up’ any residual tumor cells if they are present.
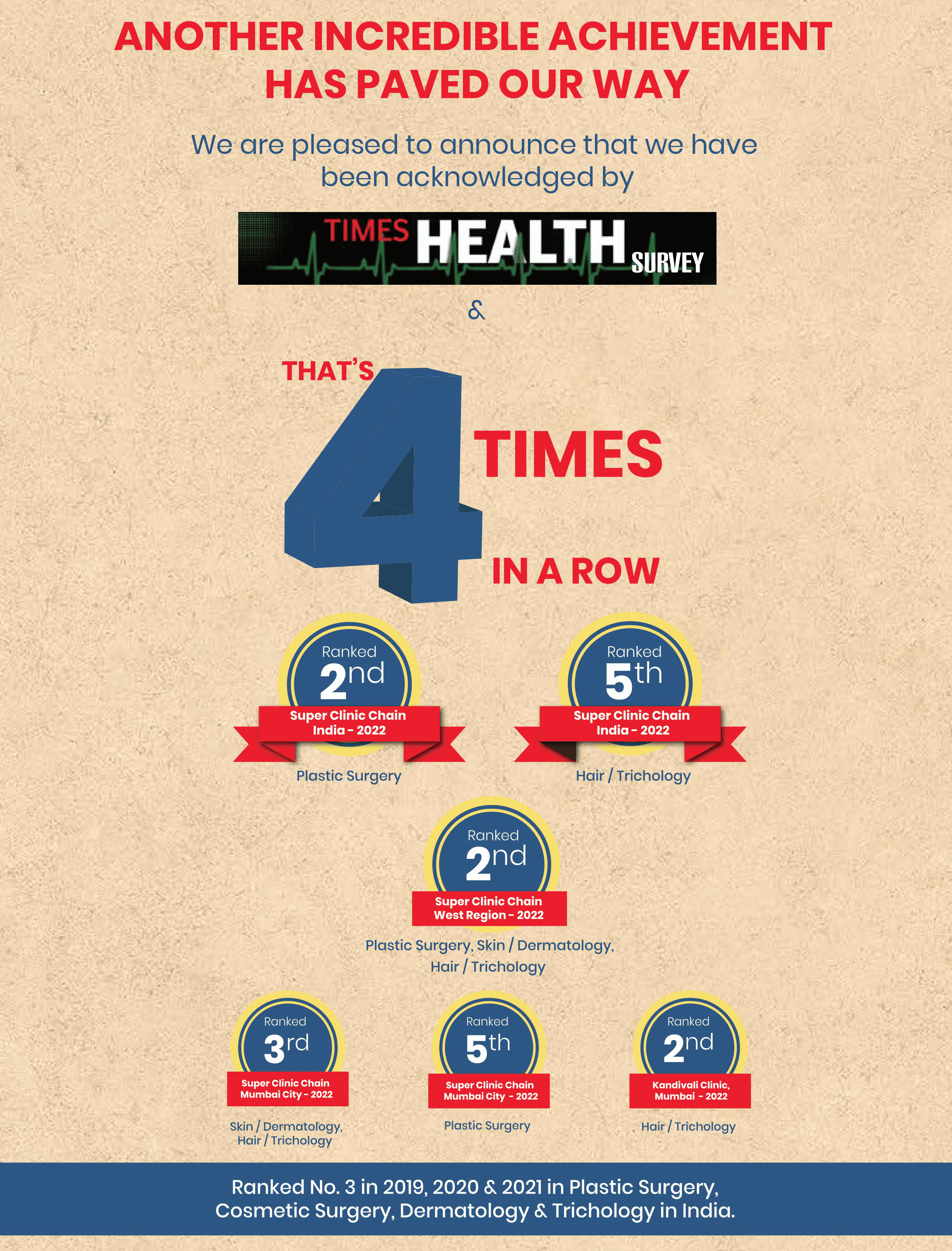
In conducting a surgical process as complicated as Orbital Exenteration, it’s important that it’s carried out by a skilled team of plastic surgeons with years of experience in the field. Surety is provided in this respect at The Esthetics Clinics, where Dr Debraj Shome — India’s Celebrity Oculoplastic surgeon with multiple honors — leads an expert staff of cosmetic surgeons and plastic surgeons. To top it off, our medical facility is equipped to ensure the success of your orbital exenteration surgery. Starting right from the pre-operative to the post-operative phases, you are greatly assured to be in safe hands.
In calculating the cost of exenteration surgery, it’s vital that we see you in person so we can offer you an accurate estimate. The magnitude of the problem, the diagnosis, the surgeon’s charge, prescriptions, and the length of follow-up affect the cost of exenteration surgery treatment. You can contact us today for a comprehensive evaluation of your case.


Dr. Debraj Shome is Director and Co founder of The Esthetic Clinics. He has been rated amongst the top surgeons in India by multiple agencies. The Esthetic Clinics patients include many international and national celebrities who prefer to opt for facial cosmetic surgery and facial plastic surgery in Mumbai because The Esthetic Clinics has its headquarters there.